The ideal reason to choose endodontic microsurgery as a treatment option is when initially all canals were located and appear to have been well treated on digital imaging. Initially unlocated canals, or inadequately treated canals, are typically best served by endodontic retreatment. Other factors that have an impact on whether endodontic surgery or retreatment is best for you is the type and how extensive the restoration presently is on the offending tooth, and the anatomic location of the tooth.
To perform endodontic microsurgery properly and successfully requires a high degree of skill. An endodontist has gone through extra training, past dental school, to acquire the advanced knowledge and skills needed to perform this highly sophisticated, technical, and microsurgical procedure. Endodontists are trained to use advanced technologies such as operating microscopes, 3D imaging, and ultrasonic instruments. A board-certified endodontist represents an individual who has undergone 3 separate, rigorous examinations to achieve the pinnacle of dentist is not needed as long as no decay (caries) is present, and your current restoration is well sealed. Over time the bone will heal, and you will have a healthy tooth.
Thorough diagnostic testing and x-ray (radiographic) imaging will be completed to ensure an endodontic problem exists and if it’s the tooth with previous root canal treatment. Additionally, Cone Beam CT 3D imaging will be required to help identify the cause of failure, and to give exact and proper measurements needed for the procedure. Your medically history will also be thoroughly reviewed. The prognosis and description of endodontic surgery will then be explained to you.
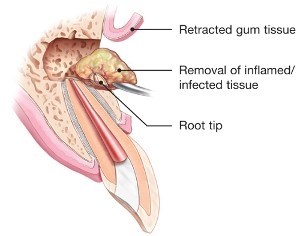
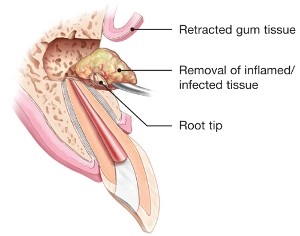
Endodontic microsurgery begins with numbing (anesthetizing) the gums (gingiva) around the tooth to ensure a comfortable and pain free appointment. An incision is made in the gums to provide access to the tip of the offending root(s). Infected and inflamed tissue is removed, biopsied, and sent to a pathologist as part of standard of care.
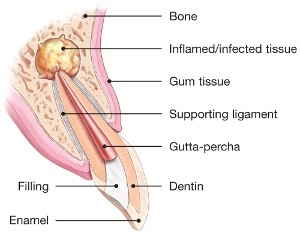
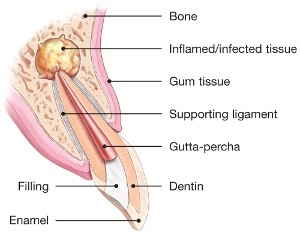

Endodontic Microsurgery (or Apicoectomy, or Root-End Surgery) is a type of dental treatment when the initial root canal treatment was not successful by either unsatisfactory healing over time, presence of persistent symptoms, or development of a new infection.
Common reasons for unsuccessful treatment include inadequately cleaned canals, additional canal(s) that were not initially treated, new decay (caries) on the tooth that leads to reinfection by bacteria of the canals. Difficult anatomy of the canals may lead to inadequate cleaning or location of the canals. Examples of difficult anatomy include very narrow (calcified) canals, curved roots, and branching canals.
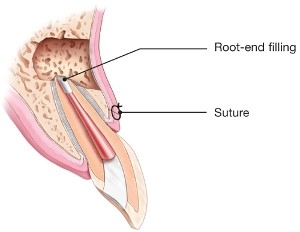
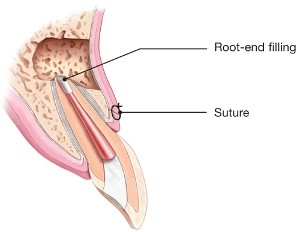
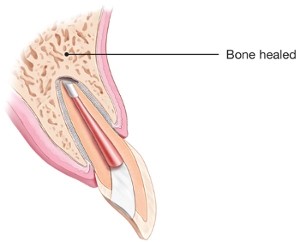
The small, infected portion of the root(s) is/are removed. Then the root(s) are prepared with small, special instruments, and then filled and sealed from the root end. Depending on the size of the infection and the amount and location of bone loss, a bone graft may be placed. The gums are then sutured back into place and post operative instructions are provided.
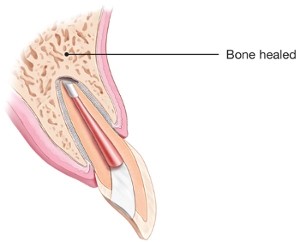
A follow-up visit is needed to remove the sutures, and evaluate the area for healing. Since endodontic surgery does not affect the top (crown) of the tooth, a final restoration by your dentist is not needed as long as no decay (caries) is present, and your current restoration is well sealed. Over time the bone will heal, and you will have a healthy tooth.
What sets endodontic microsurgery apart from traditional endodontic surgery are the advancements in and application of technology. As mentioned previously, Cone Beam CT 3D imaging provides an exact reconstruction of the surgical site and allows for precise measurements. The state-of-the-art surgical operating microscope at Buffalo Endodontics provides superior magnification and illumination of the operating field allowing for visualization of the intricate details of anatomy needed for a successful outcome. Ultrasonics and other microsurgical instruments allow for the delicate treatment and handling needed for high success. Advanced root filling materials that possess superior healing characteristics are also utilized. All of these advancements result in a more successful outcome compared to traditional endodontic surgery. Saving your natural tooth is an excellent decision, since nothing looks, feels, or functions like your natural tooth.